Medical malpractice remains a constant threat to many physicians and with good reason. From 2017 to 2021, medical malpractice claims can be classified into three primary categories.
The highest percentage of medical malpractice claims includes the following:
- 28.5% involves the improper treatment,
- 26% due to failure to diagnose, and
- 24% from surgery complications.
Research has revealed that medical errors are responsible for more than 250,000 deaths annually in the United States, positioning it as the third leading cause of death after cancer and cardiovascular diseases. The statistics drive the point further that medical malpractice continues to loom over the entire industry.
Medical Malpractice: A Problem With Multiple Solutions
Medical malpractice affects not only patients but their physicians. Unexpected outcomes can cause healthcare providers to second-guess themselves. They might experience a range of emotional responses to medical malpractice claims, including an undue sense of responsibility or guilt, genuine sorrow for those affected, and feelings of dread, anxiety, and fear of being sued.
Medical malpractice lawsuits can be emotionally taxing and require significant amounts of time and resources to pursue. However, many cases are resolved through out-of-court settlements in which both parties agree to terms, and the physician’s insurance company pays a monetary sum. Although this might offer some relief, it can be the smallest of comforts to physicians who must deal with the fallout.
Medical malpractice lawsuits can increase insurance premiums for doctors and nurses, causing them to raise fees to offset these costs. This, in turn, may prompt patients to seek more affordable alternatives, potentially resulting in a loss of business for the affected medical practice.
Providing care per industry standards can reduce malpractice cases, but patients can still file lawsuits. Physicians who actively prevent malpractice can minimize patient harm and the number of lawsuits that go to trial.
The 4 C’s of Medical Malpractice Prevention are Compassion, Communication, Competence, and Charting, and the real power might rest in charting.
Proper charting techniques can significantly reduce medical malpractice in healthcare settings while helping physicians and patients cope with rising premiums. Therefore, healthcare professionals must adopt the best charting practices available.
Why is Charting Important?
The main goal of medical charting is to ensure that patients receive adequate treatment by accurately documenting their data, physical and mental condition, medical history, and current care. This documentation can reduce medical malpractice claims and help patients and physicians determine if treatments are effective.
Medical records benefit patients and provide valuable information for future patients and medical research. They can help evaluate the quality of care and support ongoing research by providing insight into treatments, outcomes, and side effects.
Accurate and complete patient records are crucial for physicians to assess their performance and ensure that their treatment meets accepted standards. Physicians must follow the best practices for medical charting and record every procedure, treatment, and instruction.
Proper medical charting can benefit patients, physicians, and the entire medical community by ensuring patients receive the best possible care and enabling medical research to progress. Among the 3 Best Charting Practices, following the 6 Cs of Charting can produce the best results.
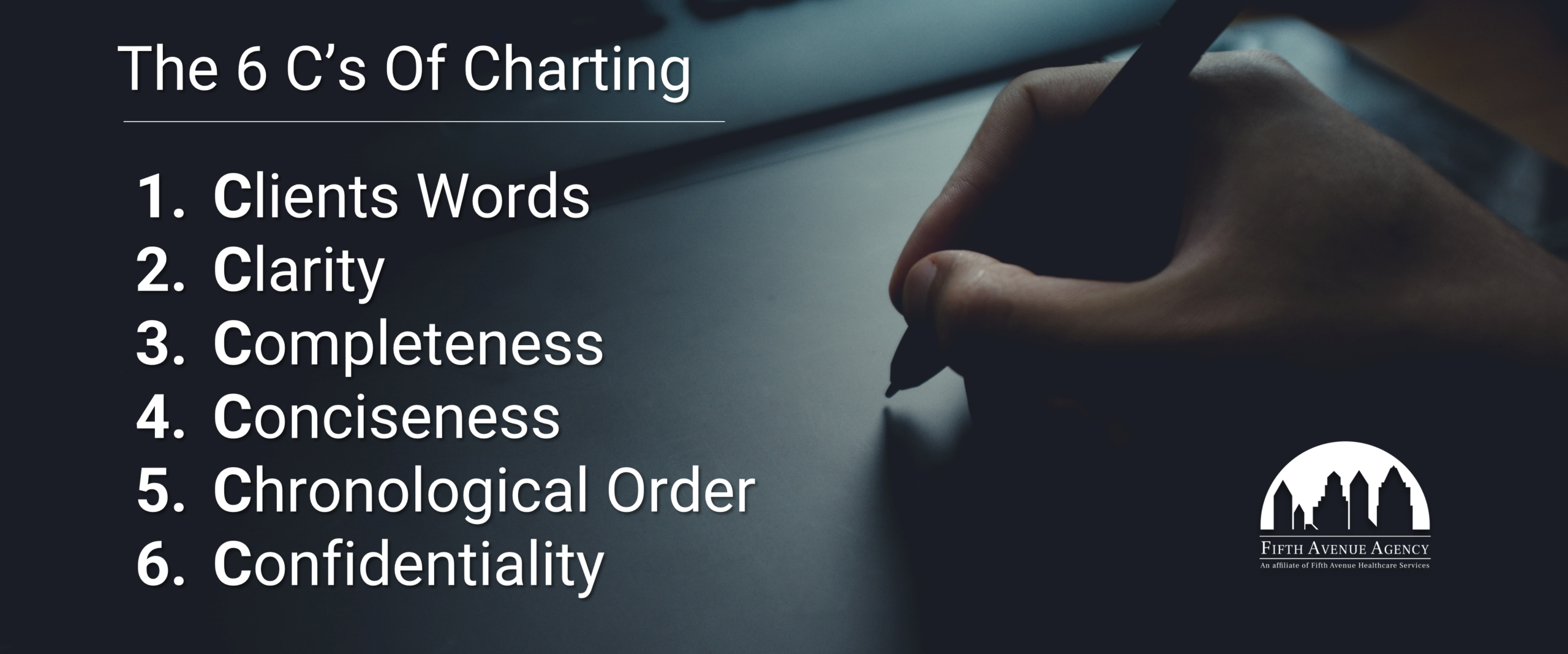
The 6 Cs of Charting include:
- Client’s Words
- Clarity
- Completeness
- Conciseness
- Chronological Order
- Confidentiality
See below for more details on each of the 6 Cs of Charting.
1. Client’s Words
When patients seek medical attention, they often present with a set of symptoms, which could range from mild discomfort to severe pain. To effectively diagnose and treat the underlying medical condition, physicians must take a detailed history from the patient. While physicians are trained to ask the right questions and perform the appropriate tests, patients can often better describe their symptoms.
Patients know their bodies best and can provide valuable insight into the nature of their symptoms. Physicians may have to make educated guesses when interpreting the patient’s symptoms, but relying solely on their interpretation can lead to misdiagnosis and improper treatment. Physicians must document the patient’s exact words when describing their symptoms.
Rephrasing or summarizing the patient’s words can alter their meaning and lead to inaccurate documentation. By accurately recording the patient’s exact words, physicians can avoid miscommunication and ensure that the patient’s concerns are being heard and addressed. This practice can lead to more precise diagnoses and better treatment outcomes.
2. Clarity
Ensuring that the language used in medical charting is consistent and universally understood is critical. Physicians should use standard medical terminology when documenting a patient’s condition. Not only does this help maintain continuity among different charts, but it also makes it easier for healthcare providers to communicate with each other about a patient’s condition.
Standard medical terminology is a language developed specifically for medical professionals to describe and communicate clinical information concisely and unambiguously. It includes terms for diagnoses, procedures, medications, and more. By using this language consistently, healthcare providers can avoid confusion and ensure that the information in a patient’s chart is accurate and precise.
Moreover, anyone with medical knowledge, not just physicians, should be able to read and interpret a patient’s chart. This includes nurses, therapists, and other healthcare professionals who may be involved in a patient’s care. By using standardized terminology, physicians can help ensure that the chart is accessible and understandable to everyone who needs it, benefiting the patient’s care.
Legibility also plays a significant part in charting clarity. People must be able to read what is written before they can understand it, so legible handwriting is critical. Smears can also obscure text and create confusion. It is recommended that the client’s words be recorded using a waterproof marker to ensure the information is not smudged or otherwise marred.
3. Completeness
Thorough documentation is crucial in providing quality healthcare to patients. It enables healthcare providers to track the patient’s condition, monitor progress, and make informed decisions on treatment options. Comprehensive documentation includes filling out all necessary forms, providing accurate medical history, and noting all crucial details of the patient’s symptoms, diagnosis, and treatment plan.
Incomplete or missing information can cause treatment delays and lead to further complications or injuries for the patient. Physicians need to take the time to document everything, including any potential risks or complications associated with treatment. This ensures the patient receives the best care possible and protects healthcare providers from litigation.

By documenting every detail, healthcare providers can establish a clear and complete picture of the patient’s health, which can contribute to better patient outcomes.
4. Conciseness
While complete documentation is essential, keeping recorded information brief and concise is equally important. This saves time and helps avoid any confusion due to lengthy and unclear records. Keeping records short makes scanning a chart quick and straightforward for physicians, nurses, and other healthcare providers. This is especially important in emergencies where every second counts. Standard terminology and abbreviations are also essential in keeping patients’ medical records concise and clear.
5. Chronological Order
Documenting events promptly is crucial for effective patient care. It helps physicians track the progression of a patient’s condition, evaluate the effectiveness of treatments and interventions, and make informed decisions about future care. In addition, accurate documentation can protect healthcare providers from legal disputes.
Dating each chart entry is especially important because it establishes a clear timeline of events. This allows healthcare providers to identify any gaps or inconsistencies in the documentation and address them promptly. When chart entries are out of order, it can create confusion and make it difficult to understand the patient’s medical history.
6. Confidentiality
Patient confidentiality is a cornerstone of medical practice. Patients have the right to expect their medical information to be kept private and confidential. Healthcare providers are responsible for ensuring that patient confidentiality is maintained at all times. Confidentiality is essential to building trust between patients and healthcare providers. Patients are more likely to disclose sensitive information to their healthcare provider if they trust it will be kept confidential.
Patient confidentiality is also a legal requirement. Healthcare providers are bound by law to keep patient information confidential. Breaching patient confidentiality can result in legal action against the healthcare provider. This can lead to loss of license, lawsuits, and other penalties.
There are several ways to maintain patient confidentiality. One way is to limit access to patient information. Healthcare providers should only access patient information on a need-to-know basis, and patient information should only be shared with individuals involved in the patient’s care.
Another way to maintain patient confidentiality is to keep patient information secure. Patient information should be stored in a safe, password-protected location.
The Perils of Poor Charting
Physicians sometimes lack an understanding of the specific information required for medical purposes. Although they may record copious amounts of information, they may fail to use the necessary terminology to achieve the highest level of specificity. Inadequate documentation can also result from time constraints, as busy physicians prioritize patient care over documentation.
Neglecting to properly document a patient’s condition, medication administration, or other aspects of their care can lead to adverse patient outcomes and create liability issues for the practice or hospital and the physician and nurse(s) in charge of the patient.
Documentation lacking clarity, specificity, or completeness is considered poor quality. Such records fail to effectively communicate a patient’s health concerns and the interventions to address them.
Examples of poor charting include:
- A lack of notes.
- Empty fields.
- Inadequate documentation of prescriptions.
- Insufficient medical history of the patient.
- Unclear handwriting.
Charting Is Only Half Of The Picture
Medical records should be reviewed to ensure the completeness of documented diagnoses and identify patient safety indicators and hospital-acquired conditions. If necessary, providers should be queried to confirm the presence of these conditions upon admission. Compliant queries should address any documentation improvement opportunities.
Education opportunities should be provided to clinicians to increase awareness of the benefits of accurate and complete documentation for patient care and their professional profiles.
Proper Charting Allows Greater Provider And Patient Protection
Charting creates comprehensive medical records that can provide a clear overview of patients’ health concerns, diagnostic assessments, and treatment plans. Accurate and detailed records also help protect physicians against potential medical malpractice lawsuits in the event of adverse patient outcomes.
Frequently reviewing charting procedures can also strengthen the integrity of records. Although charting cannot eliminate malpractice claims, it can steer physicians away from most.
More information about Fifth Avenue Agency
Fifth Avenue Agency specializes in MPLI and medical malpractice insurance, serving thousands of providers nationwide. It is part of the Fifth Avenue Healthcare Services family. Sister companies include 5ACVO (credentialing and primary source verification specialists) and Primoris Credentialing Network (credentialing and provider enrollment specialists with 54+ health plan and network provider enrollment options).
This article was initially published by Fifth Avenue Agency here. For information on Fifth Avenue Agency, please visit FifthAvenueAgency.com or Contact Us.