Companies like AVEM Health know all too well about the challenges of rural healthcare providers. Rural communities sometimes struggle with acquiring proper health care from smaller markets with fewer physicians. AVEM’s support extends to offering financial, technology, management, and capital solutions to hospitals in rural markets.
Credentialing is another challenge plaguing these markets. The obstacles blocking physicians from becoming credentialed are compounded in rural areas. Why?
This article will dive into three credentialing challenges for rural medical providers and what solutions exist to overcome them.
What is Credentialing?
Credentialing can keep patients safe, capable physicians working, and medical organizations in the business. Credentialing can confirm that a physician is competent enough to administer treatment. Since payors do not want negligent medical professionals on their plans, physicians must be credentialed before enrolling in a health plan or network option.
Credentialing involves completing approximately 52 steps before a file is ready for presentation.
Any actions resulting in oversights or mistakes could see an unqualified and unfit physician allowed to treat and possibly harm patients.
A few of the 52 steps include:
-
- Sending out, tracking, and receiving the provider application packet.
- Assessing medical malpractice claims history.
- Acquiring copies of government-issued photo ID, Malpractice, DEA, and CDS.
- Receiving an Allied Health Professional’s Supervising Physician’s Statement.
- Authenticating medical school internship, residency, fellowship, and affiliations.
- Researching primary and out-of-state licenses for disciplinary actions.
- Obtaining a copy of the provider’s current certificate of insurance.
- Performing an extensive 10-year criminal background check.
- Running a National Practitioner Data Bank query.
Why is Credentialing Important?
Without credentialing, patients could be harmed by people without the right to practice medicine. Medical malpractice can adversely affect patients’ lives and inflict financial devastation upon physicians and medical organizations.
For example, a recent malpractice verdict awarded a Minnesota plaintiff $111 million in damages. The ruling became the state’s largest medical malpractice verdict and one of the costliest in the United States. Proper credentialing might have helped the defendant avoid such a financial blow.
As previously mentioned, credentialing is also crucial to the revenue cycle. Without it, physicians cannot enroll in health plans and cannot bill payors for their services.
Credentialing challenges in any setting can upset the healthcare field on several fronts. Rural Medical America is discovering this the hard way. A rural hospital typically has more barriers to overcome than its urban counterparts.
3 Credentialing Challenges for Rural Providers
1. Rural Providers Face Limited Resources
Credentialing is usually a 52-step process that can take 90 to 120 days to complete. The process requires financial and labor resources that rural medical organizations might lack. For instance, a credentialing specialist should be hired to perform the job. Office staff can learn each meticulous step, but they might not have the time to attend to their other duties. Plus, they might not understand what to do and skip the necessary steps. A seasoned credentialing specialist should be able to do what is required to credential a physician properly.
However, a credentialing specialist does not come cheap. One can demand $72,725 per year. Factor in other costs like credentialing computer software and application fees, and rural healthcare organizations already hurting for money might not afford to credential anyone. Some might not hire office staff for regular work because the money is insufficient. It takes money to make money. Organizations cannot generate revenue without the resources to credential physicians, creating a vicious cycle where no one gets what they need. Even outsourcing credentialing to a credentials verification organization can prove difficult if there is no room in a budget to do so. Eliminating this particular challenge requires diligent efforts and a little luck.
2. Rural Providers Face A Lack of Interoperability
Interoperability is the ability of computer systems to exchange and utilize information. In healthcare settings, interoperability is a 3-pronged extension of its basic definition.
Interoperability includes:
-
- Concerns the secure sharing of digital health data without extra effort.
- Facilitates the access, exchange, and use of digital health data to authorized users.
- Bans blocking the sharing and use of digital health data.
- In effect, interoperability helps physicians deliver safe patient-centric treatments and gives patients access to their health information to manage their care better. The modes of data transmission and the policies that govern them can help the healthcare field from top to bottom. When that support does not exist, physicians and their patients cannot activate the information to better inform medical situations.
The Office of the National Coordinator for Health Information Technology found that approximately 6 of 10 rural hospitals received a digital summary of care records. 4 out of 10 rural hospitals queried health data from outside sources. One more staggering statistic belying the challenges facing rural hospitals is that they had half the rate of engaging in every aspect of interoperability (digitally finding, sending, receiving, and using) compared to suburban and urban hospitals.
Rural medical organizations suffer the most in this area due to their underfunded and understaffed natures. They cannot coordinate care for their communities if they do not have access to data that could help diagnose and treat particular illnesses. Limited resources again come into play, impacting rural medical organizations and those who rely on them.
3. Rural Providers Face Aging Infrastructure
Every industry that uses electronic systems and software has added expenses that they must include in their annual budgets. Data security and privacy programs cost money to implement and maintain. Medical information is among the most sensitive data that needs handling. The public has grown accustomed to demanding that their data be secure and accessible to authorized parties only. Healthcare organizations must make concerted efforts to meet their patient’s expectations. However, cyberattacks have failed despite the strictest security policies and procedures. Bolstering data warehouses and physical infrastructure is an ongoing burden that healthcare organizations must deal with on top of their other expenses.
Many of these organizations are becoming more vulnerable as time goes on because they cannot keep up with the financial rigors of updating their computing platforms.
Although cybersecurity threats persist, security budgets remain the same or have been slashed to cover other costs perceived as more critical. The Healthcare Information and Management Systems Society found that 50% of survey respondents said their security budgets were the same or lower in 2021 than in 2020. 39% stated that outdated technology presented a growing concern.
Although security patches and software upgrades can help prevent data breaches and other attacks, some devices and applications are no longer supported by their manufacturers because they are too old.
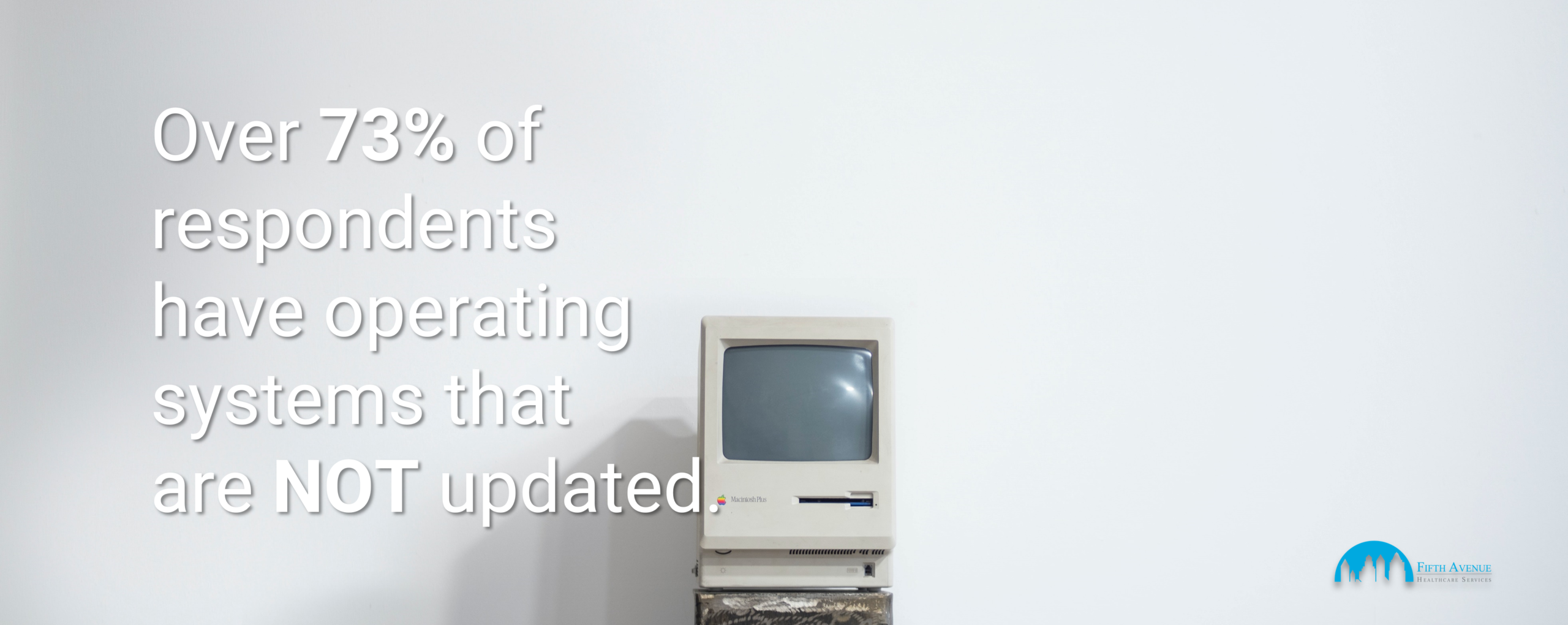
The survey above found that 73% of respondents have operating systems that are no longer updated. This alone can present significant infrastructure vulnerabilities that a software upgrade will not fix. A remarkable statistic from this survey is that 11% of respondents still have operating systems from before 2000.
Since cyberattacks are not going away, healthcare organizations must employ modern solutions to help them maintain the integrity of their cybersecurity programs. Like everything else in life, this costs money that rural areas typically do not have in abundance.
3 Additional Credentialing Challenges for Rural Providers
Bonus 1. Limited Areas Of High-Speed Internet
It should go without saying that people cannot access information online if they do not have Internet service. While some people do not have Internet service because they cannot afford it, others do not because it is simply unavailable. Rural America is often kept out of the loop because service providers sometimes do not find it cost-effective to install fiber-optic cables across vast distances to deliver service to a few subscribers. Therefore, those communities are stuck with slow Internet speeds if they have access in the first place.
The statistics present this as a more significant problem than commonly thought. In 2019, 8% of people in the United States did not have Internet access, amounting to 25 million people. Rural Americans are approximately 2X less likely to have Internet access than those living in urban areas.
What was once a luxury is now a necessity. Internet access is vital for many reasons, even in rural communities. Being left out because of location and infrastructure costs can create a considerable gap in receiving health care. Additionally, medical organizations cannot credential their physicians efficiently if they do not have reliable Internet, making patients and their doctors face this issue together.
Bonus 2. Limited Access To Smartphones and Other Devices
Even if rural communities have high-speed Internet, they must have devices to access their medical information. A 2021 study found that 80% of rural residents own a smartphone to access online patient portals and relevant apps. Although this figure is relatively high, 20% of rural residents who do not have an online-ready device cannot participate in a proactive and informed medical management plan.
Programs have been set up to help these residents pay for these devices or outright obtain them for free. However, limited access means fewer people can seek and attain the treatment they need to help ensure a better life for themselves and their families.
Rural practices and hospitals might also not have the equipment to access the Internet. As previously mentioned, many healthcare organizations, regardless of location, do not have the money to upkeep their technology adequately. Rural areas experiencing dire financial straits might be in worse positions than their suburban and urban counterparts.
Bonus 3. Limited Time
Some rural medical organizations do not have the time to work on credentialing due to staff shortages caused by problematic recruitment and retention.
The American Medical Association published a report exploring rural health physician workforce disparities in the United States. It concluded that there are not enough practicing physicians to meet the demands of rural communities. Only 12% of primary care physicians serve rural populations. 60 million+ people live in rural areas, making this shortage potentially detrimental to many. Several factors contribute to this low number, including inadequate medical training programs for rural students and a general lack of interest.
These factors also apply to healthcare professional staff. Finding skilled office personnel in these environments can prove extremely difficult. Training people to become up to speed in credentialing policies and procedures is an additional task that can weigh heavy on organizations and their employees. There might not be enough time to devote to this particular training.
Due to low staff numbers, taking time off from other duties might be impossible. There is too much work and not enough people to do it all. Add in people’s desire to move away from struggling rural communities, and credentialing is made that much harder. Organizations cannot recruit staff if the talent pool is shallow.
Conclusion: Credentialing Challenges For Rural Providers
Credentialing requires time, money, expertise, and data. These resources could be in short supply for rural medical providers, making credentialing less than an afterthought. Companies like AVEM Health, 5ACVO, and Fifth Avenue Healthcare Services can support and solve these issues. Barring any sweeping reform, credentialing challenges will remain high hurdles that must be cleared in the foreseeable future.
More information about 5ACVO
5ACVO is an NCQA Credentialing Accredited specializing in credentialing and primary source verification and is part of the Fifth Avenue Healthcare Services family. 5ACVO sister companies include Fifth Avenue Agency (MPLI and medical malpractice insurance specialists) and Primoris Credentialing Network (credentialing and provider enrollment specialists with 54+ health plan and network provider enrollment options).
For more information on 5ACVO, please visit 5ACVO.com or Contact Us.