The healthcare industry is facing a perfect storm: a nationwide shortage of healthcare workers, rising provider turnover rates, and mounting administrative burdens that strain already stretched organizations.
While many factors contribute to this crisis, one often overlooked solution can ease the burden—outsourcing healthcare credentialing. By streamlining this critical process, healthcare organizations can improve provider satisfaction, reduce turnover, and ultimately enhance patient care.
In this article, we will explore the current healthcare workforce shortage, the impact of provider turnover, and how outsourcing credentialing can be a strategic move to help organizations navigate these challenges effectively.
The Current Healthcare Workforce Shortage
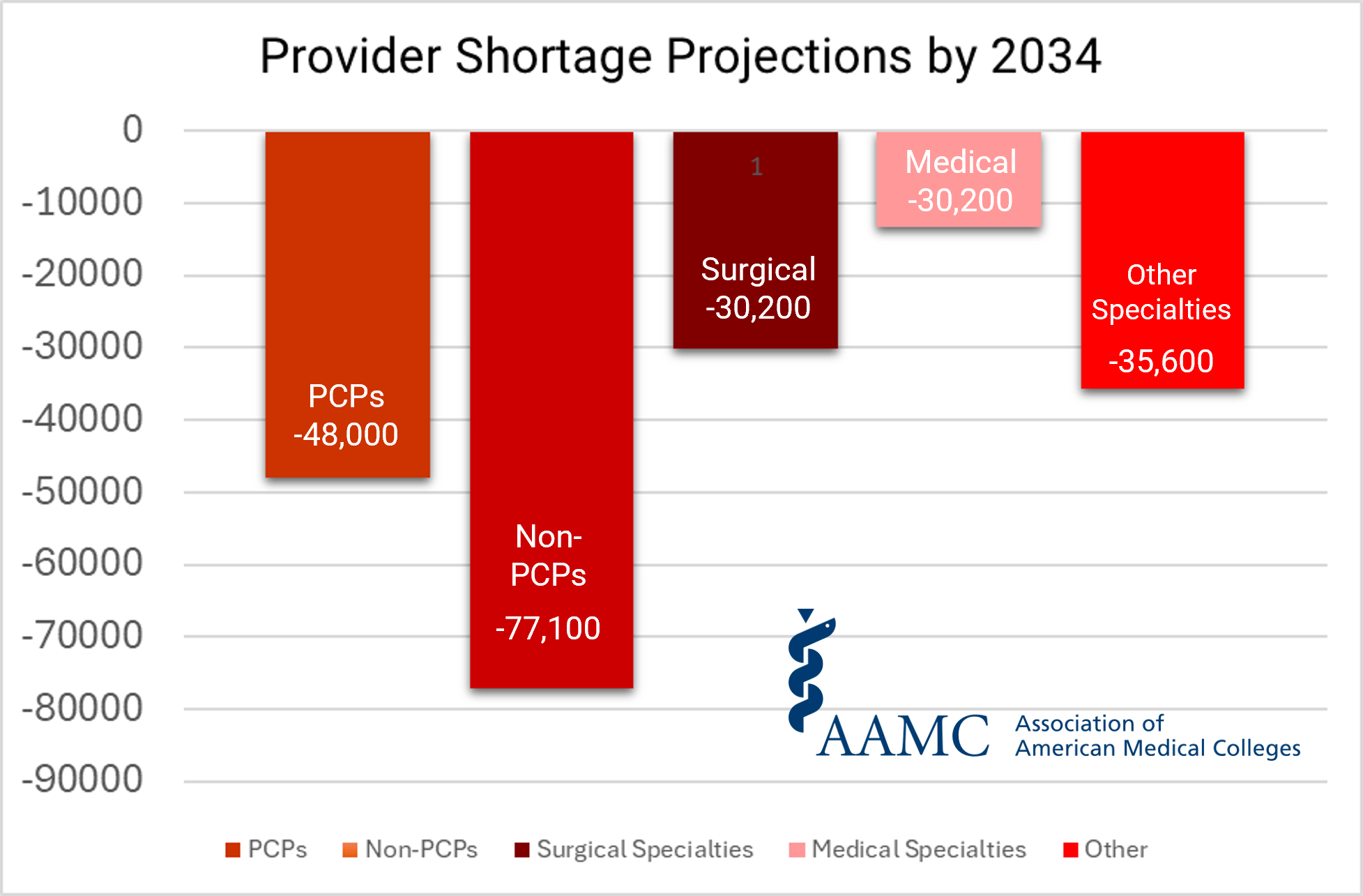
Healthcare organizations across the U.S. are grappling with an unprecedented shortage of providers, from physicians and nurses to support staff. According to the Association of American Medical Colleges (AAMC), the U.S. could face a shortage of 37,800 to 124,000 physicians by 2034. Several factors exacerbate this looming gap:
- Aging Workforce: Many healthcare professionals are nearing retirement, and the pipeline of new providers is not keeping pace. The American Nurses Association (ANA) projects that more than 500,000 seasoned RNs will retire by 2025, further compounding the staffing crisis.
- Burnout and Mental Health Challenges: The COVID-19 pandemic intensified stress levels among healthcare workers, leading to increased burnout and resignations. A Medscape National Physician Burnout & Suicide Report found that 47% of physicians reported feeling burned out in 2021, up from previous years.
- Increased Demand for Healthcare Services: An aging population and the expansion of healthcare access have driven up patient volumes, straining the existing workforce. The U.S. Census Bureau (USCB) estimates that by 2030, 1 in 5 Americans will be over the age of 65, significantly increasing the demand for healthcare services.
Adding urgency to this crisis, American Medical Association (AMA) President Jesse M. Ehrenfeld, M.D., MPH, highlighted the severity of the situation in a recent statement: “While our current physician shortage is already limiting access to care for millions of people, it’s about to get much worse.” source. This stark warning underscores the immediate need for healthcare organizations to find innovative solutions to mitigate the impacts of the shortage.
This shortage impacts not only patient care but also healthcare organizations’ operational efficiency and financial health. Delays in hiring and onboarding new providers can result in reduced patient access, longer wait times, and lost revenue.
Healthcare Provider Turnover: A Growing Concern
Provider turnover is another significant challenge. According to a 2022 report by the Medical Group Management Association (MGMA), turnover rates for physicians and advanced practice providers (APPs) reached 18%, a marked increase from previous years. High turnover rates lead to several cascading issues:
- Financial Costs: Replacing a physician can cost up to $500,000, including recruitment, onboarding, and lost revenue during vacancies. This does not account for the loss of institutional knowledge and patient relationships.
- Disrupted Patient Care: Continuity of care suffers when providers leave, affecting patient satisfaction and health outcomes. Patients often prefer seeing the same provider, and turnover disrupts this relationship, potentially leading to lower patient retention.
- Increased Workload for Remaining Staff: When providers leave, their workload often shifts to the remaining staff, leading to further burnout and potential turnover. This cycle can create a toxic work environment, exacerbating the staffing crisis.
One of the lesser-discussed contributors to provider turnover is the administrative burden—especially the credentialing process. Credentialing delays can keep new providers from seeing patients, causing frustration and financial strain.
Moreover, a slow credentialing process can deter potential hires from choosing your organization, as they may opt for employers with more efficient onboarding systems.

The Hidden Cost of Delayed Credentialing
Healthcare credentialing is a critical but time-consuming process that verifies a provider’s qualifications, experience, and licenses. While necessary to ensure patient safety and regulatory compliance, credentialing can be a significant bottleneck when not managed efficiently. According to the Council for Affordable Quality Healthcare (CAQH), the average time to credential a provider is 90 to 120 days. These delays can have serious repercussions:
- Revenue Loss: Providers who are not credentialed can’t bill insurance companies, leading to lost income. This can amount to thousands of dollars per day for a busy practice. Over a period of three months, this can lead to losses in the tens or even hundreds of thousands of dollars.
- Provider Frustration: New hires eager to start seeing patients may grow frustrated with prolonged credentialing processes, which can affect morale and increase the likelihood of turnover. Providers often cite administrative hassles as a primary source of dissatisfaction, making streamlined credentialing critical to retention.
- Impact on Patient Care: Delays in onboarding new providers contribute to longer patient wait times and reduced access to care. This not only affects patient satisfaction but can also tarnish the reputation of the healthcare organization.
- Compliance Risks: Inefficient credentialing can lead to compliance issues, putting the organization at risk of legal challenges and financial penalties if providers practice without proper verification.
When credentialing becomes a bottleneck, it affects providers and the entire organization. This is where outsourcing healthcare credentialing can offer significant advantages.

The Solution: Outsourcing Healthcare Credentialing to Ease the Burden
Outsourcing healthcare credentialing to a Credentialing Verification Organization (CVO) like 5ACVO can alleviate many of the challenges associated with in-house credentialing processes. Here’s how:
- Faster Turnaround Times: CVOs specialize in credentialing and have dedicated teams to manage the process efficiently, creating faster turnaround times. This can reduce the credentialing timeline from months to weeks, allowing providers to start generating revenue sooner.
- Reduced Administrative Burden: By outsourcing healthcare credentialing, healthcare organizations free up internal resources to focus on patient care and other critical tasks, creating a simpler administrative process. This can also reduce the need for additional administrative staff, lowering overhead costs.
- Improved Provider Satisfaction: Streamlined credentialing processes mean providers can start seeing patients sooner, reducing frustration and improving job satisfaction. A smooth onboarding process sets a positive tone for new hires, increasing the likelihood of long-term retention.
- Enhanced Compliance: CVOs stay current with the latest regulatory requirements, ensuring that credentialing processes meet all necessary standards. This minimizes the risk of compliance issues and legal challenges.
- Scalability: Outsourcing healthcare credentialing allows healthcare organizations to scale their credentialing processes up or down based on their needs, providing flexibility in an ever-changing healthcare landscape.
A study published by Becker’s Hospital Review found that healthcare organizations outsourcing healthcare credentialing experienced 25% faster onboarding times and significant reductions in administrative costs. Minimizing the friction associated with onboarding improves the bottom line and helps retain providers. Additionally, research conducted by the National Association of Medical Staff Services (NAMSS), as outlined in their Medical Service Staffing Study from September 2009, reveals that outsourcing healthcare credentialing through a Credentials Verification Organization (CVO) is, on average, 5 to 7 days faster than other methods. This finding underscores the efficiency of CVO-processed credentialing.
Real-Life Examples of Outsourcing Healthcare Credentialing Success
Many healthcare organizations have already realized the benefits of outsourcing healthcare credentialing. For instance, a large multi-specialty group in Oklahoma partnered with 5ACVO to manage their credentialing process. Before outsourcing, the group faced average credentialing times of 90 days, leading to delays in provider start dates and revenue loss. After partnering with 5ACVO, the average credentialing time was reduced to under 30 days, allowing providers to begin seeing patients sooner and improving overall satisfaction.
Another example involves a regional hospital system that struggled with high provider turnover due to administrative frustrations, including credentialing delays. By outsourcing healthcare credentialing to 5ACVO, they streamlined their credentialing process, reduced administrative burdens on their providers, and saw a 15% decrease in turnover rates within the first year.
Additionally, patient satisfaction scores improved as wait times decreased and provider continuity stabilized.
A third case study features a mid-sized surgical center that faced compliance issues due to outdated credentialing practices. After outsourcing healthcare credentialing to 5ACVO, the center improved its compliance metrics. It reduced the time spent on credentialing tasks by 40%, freeing up staff to focus on patient care and other critical functions.
These success stories highlight the benefits of outsourcing healthcare credentialing in today’s challenging healthcare landscape.
Why Now is the Time to Outsource Healthcare Credentialing
With healthcare organizations facing mounting pressure from workforce shortages and rising provider turnover, the need for efficient, streamlined credentialing processes has never been more critical. Outsourcing credentialing is no longer just a cost-saving measure—it’s a strategic move that can improve provider retention, reduce administrative burdens, and enhance patient care.
By partnering with a trusted CVO like 5ACVO, healthcare organizations can confidently navigate the workforce crisis, ensuring that providers are credentialed quickly and accurately. This helps retain top talent and ensures patients receive timely, high-quality care.
Moreover, outsourcing credentialing allows organizations to focus on what they do best—delivering exceptional patient care. In a time when healthcare providers are stretched thin, every efficiency gained can make a significant difference.
Take the Next Step: Streamline Your Credentialing with 5ACVO
If your healthcare organization struggles with staffing shortages, high provider turnover, or credentialing delays, it’s time to consider outsourcing your credentialing process. 5ACVO offers comprehensive credentialing solutions that can help you streamline operations, reduce administrative burdens, and retain your valued providers.
Visit 5ACVO.com to learn more about our credentialing services and how we can help your organization thrive. Ready to take the next step? Contact us today through our Contact Us page to see how we can customize our credentialing solutions to meet your unique needs.
Organizations can survive and thrive in this challenging environment by addressing the healthcare workforce crisis with proactive solutions like outsourced credentialing. Don’t let credentialing delays hold your organization back—partner with 5ACVO and take control of your credentialing process today.
More information about 5ACVO
5ACVO is an NCQA Credentialing Accredited company that specializes in credentialing and primary source verification and is part of the Fifth Avenue Healthcare Services family. Its sister companies include Fifth Avenue Agency (MPLI and medical malpractice insurance specialists) and Primoris Credentialing Network (credentialing and provider enrollment specialists with 54+ health plan and network provider enrollment options).
For more information on 5ACVO, please visit 5ACVO.com or Contact Us.